Worried About Prostate Cancer?
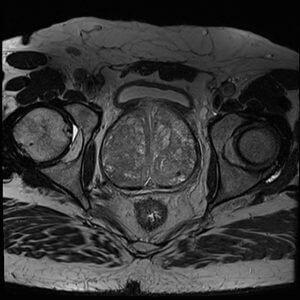
MRI can clarify whether you need a biopsy—and where to focus it.
By the Numbers:
If your doctor mentioned a possible prostate biopsy, you still have options. A prostate MRI (mpMRI) is often used first to help decide whether a biopsy is needed and, if so, where to target it. Below are key facts and smart questions to ask your urologist.
Prostate cancer is the most common cancer in U.S. men (after skin) and the #2 cause of cancer death after lung — about 1 in 8 men will be diagnosed. 1
Most men with prostate cancer don’t die from it — active surveillance and treatments are effective when cancer is found early. 1
PSA alone is imperfect: it can be high even without cancer and doesn’t show where a tumor is. 2,3. With PSA alone, hundreds of thousands of unnecessary biopsies are done every year.
MRI first can reduce unnecessary biopsies and improve targeting when biopsy is needed.4,5,6
"MP-MRI, used as a triage test before first prostate biopsy, could identify a quarter of men who might safely avoid an unnecessary biopsy and might improve the detection of clinically significant cancer." - The Lancet
Before You Biopsy: A Simple Guide for Men Over 40
Learn how prostate MRI can help you and your doctor decide if a biopsy is really needed — and often avoid one altogether.
Reviewed by imaging specialists. No spam — unsubscribe anytime.
Comparing screening tools: MRI, PSA Blood Test, and Rectal Exam
| Screening Test | Cancer Detection Rate* | False Positive Rate |
|---|---|---|
| Prostate Specific Antigen (PSA) | 21% | 76% |
| Digital Rectal Exam | 30-50% | 6-15% |
| Multi-parametric MRI | 90-93% | 25-59%** |
*For clinically significant cancer, classified as cancer that has the potential to metastasize (Gleason Score > 7)
**Note: MRI false positive rate depends on how suspicious a finding needs to be before recommending biopsy - ranging from 25% (only very suspicious findings) to 59% (including moderately suspicious findings).
Statistics compiled from the following sources: 7, 4, 8, 9, 10, 11, 12, 13


Why MRI Before Biopsy?
Prostate biopsies are invasive procedures that carry risks:
Diagnostic Limitations
Without MRI
Traditional prostate biopsies without imaging guidance are called "systematic biopsies" - typically using 12 needles that sample approximately 1% of the prostate volume
Can miss clinically significant cancer (20-30% of cases on first biopsy)
Can overdetect clinically insignificant cancer that may never cause harm
Often needs to be repeated if PSA remains elevated
35-40% of men with persistent clinical suspicion require repeat biopsy
Common Biopsy Side-effects
Blood in urine or semen (common - lasts 1-3 weeks)
Pain and discomfort (most men have mild discomfort; 5-10% need pain medication)
Infection risk (0.5-1% require hospitalization for sepsis)
Temporary urinary retention (0.2-1.9%)
MRI Shows:
Location and size of suspicious lesions
Likelihood of clinically significant cancer (PI-RADS score 1-5)
Grade and stage indicators
Enables targeted biopsy of suspicious areas (instead of systematic sampling)
Allow a targeted biopsy if needed (instead of random sampling)
Can be fused with real-time ultrasound to guide biopsy in a procedure called MRI/ultrasound fusion biopsy
Research Shows MRI is Superior
MRI detects a high proportion of clinically significant cancers; performance may vary by center and protocol.
Allows 27-42% of men to avoid biopsy entirely
Reduces detection of low-risk cancers that don't need treatment
Improves targeting if biopsy is needed
Advocate For Yourself
Don't be afraid to advocate for yourself. Here are questions to bring to your next appointment:
About MRI
Would you recommend getting an MRI before proceeding to biopsy?
What are the benefits and downsides of doing an MRI first in my situation?
Do you have experience interpreting prostate MRI results?
Where would I go for the MRI, and who would read the results?
About Biopsy
What are the risks of biopsy in my case?
If we do a biopsy, would it be targeted (MRI-fusion) or random sampling?
What happens if the biopsy is negative but my PSA stays elevated?
About Your Specific Situation
Given my age, PSA level, and family history, what are my options?
Can we do active surveillance instead of immediate biopsy?
What would you recommend if this were your father/brother?
Remember: Your urologist wants what's best for you. Most will appreciate informed patients asking good questions.
MRI FAQ
Your Next Steps
Talk to Your Urologist. Bring this information to your next appointment. Use the questions above to discuss whether MRI-first makes sense for your situation.
Find an MRI Center. Look for imaging centers with radiologists experienced in prostate MRI. Verify insurance coverage before scheduling.
Stay Informed About Prostate Health
Get updates on:
New advances in prostate screening technology
How to access MRI-first screening in your area
Expert guidance on navigating your prostate health journey
We respect your privacy. Unsubscribe anytime. No spam.
Have questions about prostate health or screening options? Subscribe above and email us at [email protected]. We're here to help.
About This Resource
This educational resource was created to help men make informed decisions about prostate cancer screening. We are not medical professionals and this information is not medical advice. Always consult with your urologist before making decisions about your health.The information here is based on published medical research, clinical guidelines from major urology organizations, and current standards of care.
Who Created This Resource?
This educational site was created by a medical device company founded by PhD MRI experts. We are working on developing new types of MRIs, and we collaborate closely with leading urologists and radiologists at major academic medical centers.We're developing portable MRI technology to make prostate screening accessible and affordable for the 4-5 million men annually with elevated PSA results. Our goal: make MRI-first screening the gold standard.We're not selling anything yet - we created this free resource to help men make informed decisions today while we work to transform prostate cancer screening for tomorrow.